
laparoscopy and laser Centre

laparoscopy and laser Centre
Proctology also known as anorectal surgery is a branch of medicine that deals with the diagnosis and treatment of diseases of colon, anus and rectum . It is best to consult with our proctologist with more than 18 yrs of experience who can evaluate your specific condition and recommend the most appropriate surgery options available.
LAPSER is a BEST LASER SURGERY HOSPITAL IN CHENNAI which aims to deliver a hassle-free surgical experience to all patients by cutting edge technology available in market.
| Open Surgery | Laser Treatments | |
|---|---|---|
| Cuts | Multiple | Minimal |
| Scars & Stiches | Multiple | Minimal |
| Procedure | Painful | Minimal Pain |
| Blood Loss | High | Minimal |
| Infection Chances | High | Minimal |
| Recovery | Bed Rest Required | Fast Recovery |
| Hospital duration | Long | Short |
| Technology | Outdated | Most Advanced |



Laser treatment is beneficial for patients suffering from piles , fissure , fistula and pilonidal sinus. It is minimal invasive and helps in speedy recovery for patients
Yes, it is completely safe to visit Lapser clinic or hospital. Lapser has placed the highest standards of safety and hygiene practices while treating or diagnosing any patient. Lapser has arranged for temperature screening at the gates of every clinic and hospital.
Anorectal surgery refers to surgical procedures performed in the area of the anus and rectum. Diseases involving anorectal region are fissure , haemorrhoids ,fistula & rectal prolapse
Hemorrhoids (HEM-uh-roids), also called piles, are swollen blood vessels in anus and lower rectum. Hemorrhoids developing inside the rectum is (internal hemorrhoids) or under the skin around the anus (external hemorrhoids).
Nearly three out of four adults will have hemorrhoids from time to time. Hemorrhoids have a number of causes, when a person constantly exerts pressure in and around the areas of anus and rectum due to several reasons like constipation or in loose stools, the blood vessels around those parts swell and bulge, forming piles. Also, in case of constant straining, the veins might get engorged, enlarged and wider with more blood than usual leading to the formation of one or more piles.

Signs and symptoms of hemorrhoids usually depend on the type of hemorrhoid.
Internal hemorrhoidsare present inside the rectum hence can't beseen, and rarely cause discomfort. Appears on straining when passing stool.
Bleeding per rectum or haemorrhoids that don't improve after a week of home care.
Don't assume rectal bleeding is due to hemorrhoids, especially if you have changes in bowel habits or if your stools change in color or consistency. Rectal bleeding can occur with other diseases, including colorectal cancer and anal cancer.
Seek emergency care if you have large amounts of rectal bleeding, light headedness, dizziness or faintness.
An anal fissure is a tear in the thin, moist tissue (mucosa) that lines the anal canal. It may occur when you pass hard or large stools. Anal fissures typically cause pain and bleeding with passage of stool.
Medical history and a physical examination, including a gentle inspection of the anal region helps in visualise the tear .Usually this exam is all that's needed to diagnose an anal fissure.
An acute anal fissure is a fresh tear. A fissure is considered chronic if it lasts more than eight weeks.A chronic anal fissure likely has a deeper tear, and may have internal or external fleshy growths.
An anal fistula means a small tunnel that occurs or develops between the skin near the anus and bowel (where poop leaves the body). In simple terms, they are just the result of an infection near the skin of the anus causing a collection of pus in the surrounding tissue. Most of the time it is the result of the infection in a gland that spreads to the skin whose symptoms involve swelling, pain, blood discharge, or pus from the anus.

When there is an abnormal connection between the perennial skin and the epithelialized surface of the anal canal.
The abnormal openings or connections between the urinary tract organ with another organ or within the urinary tract organ.
There are many other types of fistulas such as: Colocutaneous fistula or Enterocutaneous develops between the skin of the colon and the small intestine. Enteroenteral fistula develops among two parts of the intestine.
If you have any of the mentioned symptoms or signs of an anal fistula or when you have a previous anal problem or abscess. You must consult your doctor because he or she will be the only one who can provide you with the right guidance and help you get rid of this fistula.
A pilonidal sinus is a chronic skin condition that can cause irritation, pain, and even infection. These pockets of pus are most commonly located near the tailbone but can also appear around other areas like the inner thighs or buttocks.
Pilonidal sinuses form when hair grows into the skin and becomes trapped under your skin. This causes inflammation to develop, resulting in an infection known as folliculitis. Folliculitis is often mistaken for acne because it looks similar on your skin’s surface (whiteheads and blackheads). The difference between folliculitis and acne is that folliculitis occurs when bacteria grow inside of your hair shafts, while acne occurs when bacteria grow on top of your skin’s surface, causing pimples or whiteheads.
You may not have any noticeable symptoms at first other than a small, dimple-like depression on the surface of your skin. However, once the depression becomes infected, it will quickly develop into a cyst (a closed sac filled with fluid) or an abscess (a swollen and inflamed tissue where pus collects).
You may also experience a low-grade fever, but this is much less common.
If your case is diagnosed early on, you aren’t experiencing severe pain, and there’s no sign of inflammation, it’s likely that your doctor will prescribe a broad-spectrum antibiotic. A broad-spectrum antibiotic is an antibiotic that treats a wide range of bacteria. It’s important to realize that this won’t heal the sinus tract, but it will give you relief from the infection and discomfort. Your doctor will recommend that you get a follow-up exam, regularly remove hair or shave the site, and pay particular attention to hygiene.
This procedure alleviates symptoms from an abscess, or a collection of pus inside the sinus. Before this procedure, your doctor will give you a local anesthetic. They will then use a scalpel to open the abscess. They will clean away any hair, blood, and pus from inside the abscess.
Your doctor will pack the wound with sterile dressing and allow it to heal from the inside out. The wound usually heals within four weeks, and many people don’t require any further treatment.
For this type of treatment, your doctor will first give you a local anesthetic. They will then inject phenol, a chemical compound used as an antiseptic, into the cyst. This procedure may need to be repeated several times. Eventually, this treatment will cause the lesion to harden and close.
This treatment has a very high recurrence rate. Therefore, it’s uncommon in the United States. Doctors turn to surgery as the treatment of choice in some cases.
If you have a recurring PNS or if you have more than one sinus tract, your doctor will recommend a surgical procedure.
You will first be given a local anesthetic. Then, the surgeon will open the lesions, removing all of the pus and debris. Once this process is complete, the surgeon will stitch the wounds closed.
After surgery, your doctor will explain how to change the dressings and will recommend shaving the site to prevent hair from growing into the wound.
People have pilonidal sinus, they may have discomfort and irritation around the tail bone area at this time they can consult with a doctor at the beginning stage itself.
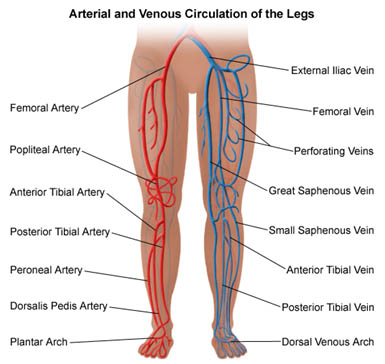
Varicose veins are dilated, tortuous, elongated veins that is close to the skin's surface (superficial) .The blood moves towards the heart by one-way valves in the veins. When the valves become weakened or damaged, blood can collect in the veins. This causes the veins to become enlarged. Sitting or standing for long periods can cause blood to pool in the leg veins, increasing the pressure within the veins. The veins can stretch from the increased pressure. This may weaken the walls of the veins and damage the valves.

Varicose veins may be more common in some families (inherited). Increased pressure in the veins may cause varicose veins. Factors that may increase pressure include:
varicose veins can cause aching pain and discomfort. Sometimes varicose veins lead to more-serious problems.spider veins are a common& mild variation of varicose veins — are more of cosmetic concern.
Spider veins are similar to varicose veins, but they're smaller. Spider veins are found closer to the skin's surface and are often red or blue. They vary in size and often look like a spider's web.
Your health care provider will do a physical exam, including looking at your legs while you're standing to check for swelling. Your provider might also ask you to describe pain and aching in your legs.
In addition to a complete medical history and physical exam, diagnostic procedures for varicose veins may include:
Duplex ultrasound. A type of vascular ultrasound done to check blood flow and the structure of the leg veins. Duplex means two types of ultrasound are used.
Medical treatment may not be necessary if there are no symptoms. However, varicose veins may sometimes worsen without treatment.
Varicose veins are usually not serious. But, complications may happen. They include:
Steps to prevent varicose veins include:
If you're concerned about how your veins look and feel and self-care measures haven't helped, see your health care provider.